Pancreatic ductal adenocarcinoma (PDAC) is one of the deadliest cancers, with 5-year survival rates historically around 10%. Pancreatic cancer develops slowly from known precursor lesions (pancreatic intraepithelial neoplasms, PanINs) in the ductal system and is often diagnosed late after distant metastases are present. While the incidence of pancreatic cancer in the general population is low, some people are of at increased risk for development of PDAC due to family history or presence of certain mutations.
In the Kiemen lab we study the microanatomy of the normal pancreas, the morphology, immune microenvironment, and genetic features of PanIN lesions in sporadic cases and high-risk individuals, and the 3D invasion patterns of pancreatic cancer.


PanINs (pancreatic cancer precursor lesions)
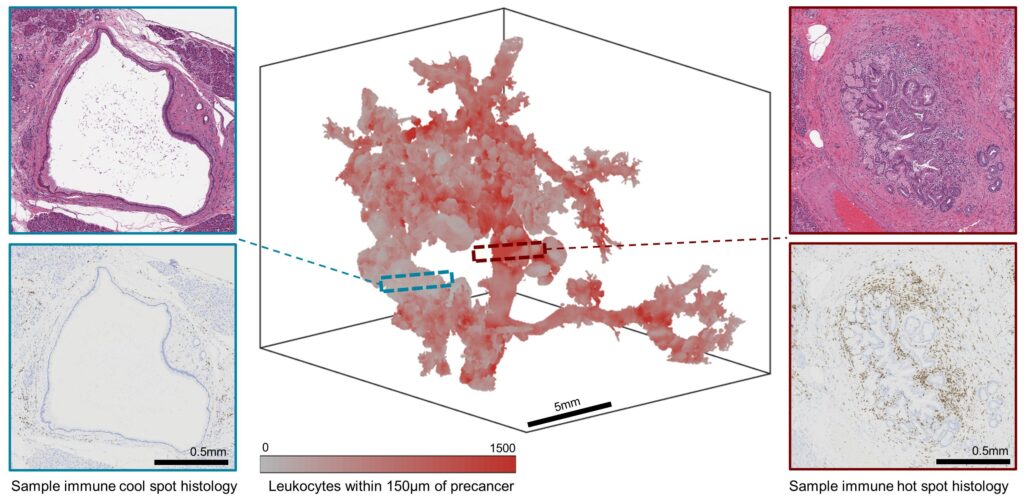
PanINs are microscopic, mucinous cysts that develop in the pancreatic ducts of individuals and can spontaneously develop into pancreatic cancer. While recent evidence suggests that PanIN are significantly more common than previously believed, (1, 2) the incidence of PDAC remains quite low, suggesting that most PanIN will never progress to cancer. Using 2D and 3D pathology, we interrogate the incidence and microanatomical qualities of PanIN lesions in human tissues to try to identify characteristics of PanIN at high risk of progression.



Pancreatic cancer invasion
Pancreatic cancer often presents as small, but highly branched, tumors. In two dimensions (single histological sections) this may appear as groups of small clusters of cancer cells, but in three dimensions these clusters are often connected. Pancreatic cancer invades distally along structures such as aligned collagen fibers, externally and internally along the vasculature and lymphatic vessels, and along the nerve fibers.

